PANDAS: A Treatable Condition

Paediatric Autoimmune Neuropsychiatric Disorder associated with group A Streptococcus (PANDAS), is a condition seen in the paediatric population consisting of tics or obsessive compulsive disorder exacerbated or brought on by a common bacterial infection called Group A streptococcus (GAS). This infection may initially present with a sore throat or chest infection with the subsequent onset of neuropsychiatric symptoms (tics and obsessive compulsive behaviours). The disease sits under a bigger umbrella term “PANS” which stands for Paediatric Acute-onset Neuropsychiatric Syndrome. The term PANS/PANDAS and immune mediated behavioural change are often used interchangeably.
The Children’s e-Hospital regularly treats patients with PANDAS and the PANS PANDAS service is under regular audit to ensure that we provide the best care for our patients. Our latest audit in August 2022 showed that nearly 9 out of 10 of our patients achieved a good, very good or excellent response to our treatment regimes. There were no significant adverse effects reported and our patient satisfaction rates are very high. We are a CQC registered service and our last inspection rated us as an “Outstanding” service.
This group of disorders has been given ICD-11 code 8E4A.0 by the World Health Organisation but despite this an audit done by The Children’s e-Hospital showed that 90% of GP’s were unfamiliar with this condition.
Recent work by the PANS PANDAS Working Group (working with the BPNA, The Royal College of Paediatrics & Child Health, The Royal College of Psychiatry, The Royal College of Nursing, The Royal College of Occupational Therapy, The British Paediatric Allergy, Infectious disease and Immunology Group, PANS PANDAS UK and Social workers) has led to the publication of a unified statement to counter the previous consensus statement which led to the restrictions in the provision of care to children with PANS PANDAS. This is an important step forward in the development of a UK based treatment protocol with all major specialities represented.
PPWG Statement 24 February 2023
This group of disorders is thought to occur after the body produces an antibody to fight a common everyday infection. This antibody then goes on to stimulate a part of the brain called the basal ganglia which is involved with movement control (or regulation of obsessive compulsive behaviours) and this results in the abnormal movement, feeling or compulsion that the patient experiences.
PANS (Paediatric acute-onset neuropsychiatric syndrome) describes a clinical syndrome that may be caused by noninfectious or infectious triggers. Proposed diagnostic criteria for PANS include: the sudden onset of OCD or severely restricted food intake, severe neuropsychiatric symptoms (eg, anxiety, depression, emotional lability, etc) or symptoms not better explained by a known neurologic or medical disorder. The key words in this are “sudden onset”. Symptoms appear dramatically and there is a rapid shift in the child’s behaviour.
Background
Rheumatic fever has been a less commonly recognised condition over the past 30-40 years. Part of the diagnostic criteria for rheumatic fever included a condition called “Sydenham’s chorea” or ‘St. Vitus dance” . This was an abnormality of movement which was associated with streptococcal infection. Individuals diagnosed with rheumatic fever were given long term prophylactic penicillin to treat the condition and prevent disease relapse.
Dr Susan Swedo during her research into Sydenham’s chorea realised that there were a sub-group of patients with tics & obsessive-compulsive behaviour that had a sudden onset of symptoms. This was very different to the movements seen with rheumatic fever. Crucially the symptoms had a very rapid pace of onset.
Signs & symptoms
PANDAS symptoms typically start abruptly, almost as if a switch has been thrown. Symptoms include tics, sleep disturbance, obsessive compulsive behaviour, deterioration in handwriting, eating disorders (including anorexia but the problems appear to be more centred on difficulty in coordinating swallowing), behavioural regression and urinary incontinence. By definition these occur following a streptococcal infection which then results in the stimulation of antibodies which stimulates the part of the brain involved in movement and behaviour regulation (the basal ganglia). Examination of the child reveals a child who is “trapped” or “psychologically burdened”. They may have reduced muscle power and may show abnormal movements.
Pediatric Acute-onset Neuropsychiatric Syndrome (PANS) is defined by the rapid onset of obsessive–compulsive disorder (OCD) or eating restrictions and co-morbid symptoms from at least two of seven categories:
- Anxiety (particularly separation anxiety)
- Emotional lability or depression
- Irritability
- Aggression, and/or severely oppositional behaviours
- Deterioration in school performance related to ADHD-like behaviours, memory deficits, and cognitive changes
- Sensory or motor abnormalities
- Somatic signs and symptoms, including sleep disturbances, enuresis, or urinary frequency (Swedo et al. 2012; Chang et al. 2015). Acute onset cases that are triggered by Group A streptococcal infections may meet diagnostic criteria for both PANS and PANDAS.
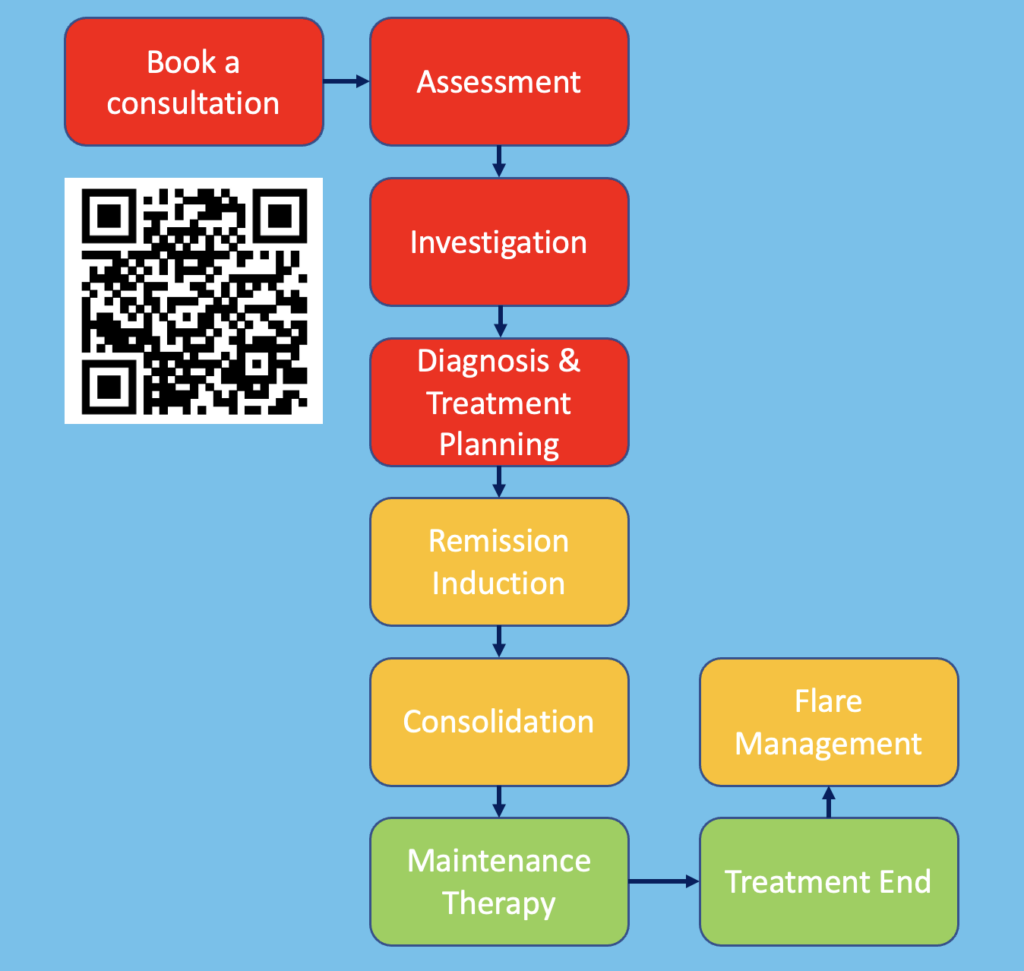
The Children’s e-Hospital PANDAS Clinical Model
The Children’s e-Hospital PANDAS Model has been determined by analysis of patients with PANDAS who were treated by The Children’s e-Hospital. This data and model were presented at the SANE PANS/PANDAS conference in Malmo, Sweden in October 2019.
The Children’s e-Hospital approach to treating patients with PANS PANDAS
Diagnosis
Criteria for diagnosis of PANDAS include:
- Presence of OCD and/or Tics
- Pre-pubertal onset
- Acute onset of symptoms with an episodic pattern
- Association with a neurological abnormality
- Temporal relationship with Group A strep infection (Determined by a raised ASO titre, Anti-Dnase B or isolation of group A streptococcus from a throat or skin swab).
Examination of the child should include looking at the throat, ears, skin (eg for impetigo or guttate psoriasis), examining the peri-anal area and genitals for infection, checking for a heart murmur and assessing weight and height.
Investigations
Having the right investigations to approach the management and treatment of a child with PANDAS is essential. Our experience has shown that there is variability between laboratories and that using the right laboratory is important. The investigations that we recommend are available to health care professionals through our Virtual Medical School (postgraduate section). It is important to look at the child as a whole and aim to optimise the health of the child. This will include looking at conditions such as allergy.
Disease monitoring
The Children’s e-Hospital Integrated PANDAS Scoring (CHIPS) system uses a combined electronic modification of the CY-BOCS (Children’s Yale Brown Obsessive Compulsive Scoring System) and the Yale Tic Scoring system to allow us to quantify and monitor the response to treatment. This allows us to ensure that we are implementing the right interventions for your child. Assessments are undertaken at baseline and 2 weeks, 6 weeks and 12 weeks after starting treatment.
You can also download a symptom diary by clicking on the following link; PANDAS symptom monitoring chart .This scoring sheet also allows parents to record their child’s symptoms and response to treatment and add detail such as whether or not a child is receiving antibiotics or anti-inflammatories. This information is invaluable in assessing the patients that we see using the Children’s e-Hospital on-line service but can also be used to help parents with any health professionals they see.
Treatment of PANDAS
Treatment of a child with PANDAS must be evidence led. Treatment requires efficient interfacing between different health professionals which may include GP’s, paediatricians, paediatric immunologists, paediatric neurologists and psychiatrists. It is important that all aspects of a child’s health are considered when a treatment plan is formulated. Treatment usually involves a combination of anti-inflammatory, anti-microbial, psychological and psychiatric therapies. The latter will also include behaviour modification therapies such as CBT and CBiT.
There are a number of treatment protocols that are available and which should be consulted by health professionals who have an interest in treating patients with PANS PANDAS.
- Nordic Guidelines
- JCAP Guidelines & others
These guidelines can be accessed by using the following QR codes;
Nordic Guidelines

Other Guidelines via EXPAND

Cognitive behaviour therapy (CBT)
The onset of PANDAS or PANS symptoms can be extremely distressing for the child and family members. It is therefore essential that psychological support with cognitive behaviour therapy (CBT) is initiated at an early stage. On-line CBT in children has been shown to be more effective than face to face therapy and also allows flexibility in seeking consultations. Using CBT gives parents the tools to manage their child during a crisis. We now offer an online CBT service which can be booked by scanning the QR code below.

Comprehensive Behaviour Therapy for Tics (CBiT)
CBiT is a therapy that is used to teach people with Tic’s ways to manage them. It is not a cure for tics, but it has been proven to help reduce the number, severity and impact of tics.
The success of CBIT comes from the comprehensive combination of therapies used within treatment, these consist of Psycho-education, Self-awareness training, Relaxation training, Establishing a tic hierarchy, selecting a target tic and reverse engineering it, Formulating a competing response to the target tic using habit reversal techniques, and Social support. CBIT is recommended as a first line intervention for tics by the American Association of Neurology.
The main component of CBiT is Habit Reversal Therapy (HRT). A second method is called Exposure Response Prevention (ERP). The main aim of ERP is for you to learn to tolerate the urge that comes before a tic, by learning to tolerate the urge you are learning to suppress the tic. This can also be hard work, and an uncomfortable sensation to begin with but with lots of practice it gets easier. By exposing your tics, you practice resisting the urge for longer and longer periods of time, until you can stop it in most situations for a period of time. Evidence suggests that ERP is as effective as Habit Reversal Therapy. ERP is best suited to individuals who have a range of troublesome tics or are young. Tic reduction is the result.
Maintenance therapy
Once disease remission has been achieved the antibody level will gradually fall and symptoms will slowly improve unless the immune system is re-stimulated eg with another infection.
Long term antibiotic use is not without consequence. It is important to limit the amount of antibiotic that your child receives to a minimum, thus avoiding problems such as clostridium difficile infection.This must be coordinated with the help of your GP, neurologist or paediatrician. The practice in the United Kingdom is much more conservative compared with the US and there is much more emphasis on antibiotic stewardship.
Parent support
Within the UK there is amazing support from The PANS PANDAS UK Charity who are leading the way in providing support and direction to patients and parents of children with PANS PANDAS. We would strongly recommend that you connect with this organisation if you have a child with PANS PANDAS and need support.



